Effective Ways to Treat and Manage Hypocalcemia
Mild hypocalcemia that has low concentrations of calcium in the blood produces symptoms such as muscle spasms, weakness, and even dangerous symptoms such as abnormal heart beats if not treated. Prevention of such complications is achievable, with high levels of management and treatment required to maintain a general health status. Some of the causes of hypocalcemia include; deficiencies in diet, certain illnesses or diseases, and some medicines that you may be taking. Knowledge of its causes and measures to reduce recidivism can make a tremendous positive impact on the results.
Common Symptoms and Signs
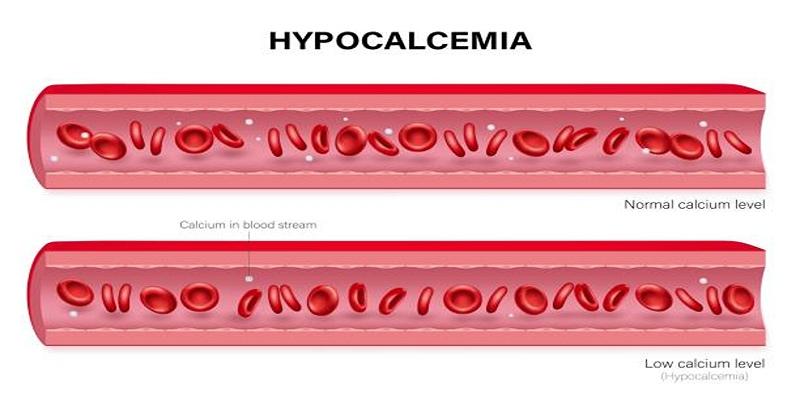
Hypocalcemia presents itself through a range of symptoms that vary in severity depending on the underlying cause and duration of the condition.
Neuromuscular Symptoms
The most frequently associated sign of hypocalcemia is neuromuscular irritability. These side effects may include muscle cramps, spasms, or stiffness in the muscle of the hands and feet. It has severe conditions that cause tetany, where stiffness and muscle spasms occur in the body cause severe pain in muscles.
Cardiovascular Symptoms
Cardiovascular effects of hypocalcemia are especially significant because hypocalcemia can induce serious cardiovascular problems. It may lead to irregular heartbeats or arrhythmias that are can severe and even fatal if not well addressed. Also, hypocalcaemia interferes with the strength of cardiac muscles and may lead to hypotension and in severe cases heart failure.
Psychological and Cognitive Effects
Low calcium levels can also impact mental health and cognitive function. Symptoms may include anxiety, depression, confusion, memory issues, or irritability. These changes are often linked to imbalances in neurotransmission caused by insufficient calcium in the central nervous system.
Bone and Dental Issues
It is a chronic condition proven to have an impact on bone health leading to osteomalacia or osteoporosis. People may also have brittle or weakened bones, more so they will easily develop fractures. It may also affect dental health with some children experiencing slow development of teeth and in adult patients, weak enamel on the teeth might be developed.
Risk Factors and Prevalence

Hypocalcemia is often caused by a deficiency of calcium in the body, which may be due to low intake through diet or impaired absorption. Individuals who are lactose intolerant or follow strict vegan diets are also at higher risk for hypocalcemia.
Risk factors for developing hypocalcemia include:
- Vitamin D deficiency
- Chronic kidney disease
- Certain medications such as diuretics and anticonvulsants
- Eating disorders
The prevalence of hypocalcemia varies across different populations, but it is more common among older adults, postmenopausal women, breastfeeding women, individuals with gastrointestinal conditions that affect nutrient absorption, and those with a history of thyroid disorders.
Diagnosis of Hypocalcemia
Hypocalcemia is diagnosed through a combination of clinical evaluation and laboratory investigations, which help identify its underlying cause and severity.
Clinical Symptoms
The clinical presentation of hypocalcemia can vary widely, ranging from mild to severe symptoms. Common manifestations include numbness, tingling sensations, muscle cramps, and spasms, particularly in the hands and feet. Severe cases may lead to tetany, seizures, or cardiac arrhythmias, requiring immediate medical intervention. Recognizing these signs early can aid in prompt diagnosis.
Laboratory Tests
Laboratory evaluations play a pivotal role in diagnosing hypocalcemia. Blood tests are conducted to measure total and ionized calcium levels. Additionally, associated markers such as parathyroid hormone (PTH), magnesium, albumin, and vitamin D levels are assessed to determine potential causes. Correcting for any deviations in these markers helps pinpoint the source of calcium imbalance.
Differential Diagnosis
Differentiating hypocalcemia from other conditions with similar symptoms is essential. For instance, hypokalemia and neurologic disorders may present with muscle weakness or spasms, mimicking hypocalcemia. By considering the patient's medical history and performing a thorough clinical and laboratory assessment, clinicians can distinguish hypocalcemia from other conditions and formulate an accurate diagnosis plan.
Treatment Approaches
Treating hypocalcemia involves addressing the cause and restoring normal calcium levels through appropriate interventions.
Acute Hypocalcemia Management
For acute symptomatic hypocalcemia, intravenous calcium is required. Calcium gluconate or calcium chloride is typically given through a slow IV infusion to avoid cardiac complications. Monitoring heart rhythm and serum calcium levels during infusion is essential.
Chronic Hypocalcemia Management
Chronic hypocalcemia is often treated with oral calcium supplements and vitamin D, which helps improve calcium absorption. Addressing underlying conditions like hypoparathyroidism or kidney problems is key to long-term management.
Dietary Adjustments
Encouraging calcium-rich foods such as dairy, leafy greens, and fortified alternatives can help maintain stable calcium levels. Nutrition counseling ensures a balanced intake of essential nutrients for bone and overall health.
Long-Term Management Strategies
Managing calcium-related conditions effectively requires a comprehensive, multidisciplinary approach. The following strategies are key for sustained health outcomes:
Lifestyle Modifications
Lifestyle changes are essential for maintaining calcium balance and bone health. Regular weight-bearing exercises, like walking or strength training, can improve bone density. Quitting smoking is also important, as both can negatively affect calcium absorption and bone strength.
Medication Management
When needed, medications play a critical role. Calcium and vitamin D supplements may correct deficiencies, while drugs like bisphosphonates are often prescribed for osteoporosis. Regularly reviewing treatment effectiveness and ensuring adherence are vital for success.
Patient Education
Educating patients about their condition and treatment helps ensure long-term success. Clear advice on diet, exercise, and medications empowers patients to take an active role in their care, reducing anxiety and improving quality of life.
Addressing Comorbidities
Effective management of related health issues, such as kidney disease or hormonal imbalances, is essential. Collaboration between primary care providers and specialists ensures tailored, coordinated care. Early detection and treatment of comorbidities can prevent complications and improve outcomes.
Conclusion
Bone health is a critical component of overall well-being, yet it is often overlooked until issues arise. Conditions like osteoporosis can lead to fractures, reduced mobility, and diminished quality of life, emphasizing the importance of prevention and early intervention. A combination of a balanced diet, appropriate exercise, and regular medical check-ups forms the foundation of maintaining strong, healthy bones. Understanding the role of nutrition, effective treatment options, and the management of comorbidities is key to addressing bone health concerns and promoting long-term strength and resilience. This guide explores essential strategies for optimal bone care.